Safety of Live donors in Living donor liver transplant: Near zero to zero mortality says This Data!
The guiding principle in living donor transplants work on the “principle of double equipoise” which says the risk to the donor must be balanced with the benefits to the recipient. It essentially means the risk to the live donor must be kept minimum and the benefits to the recipient should be aimed at the maximum.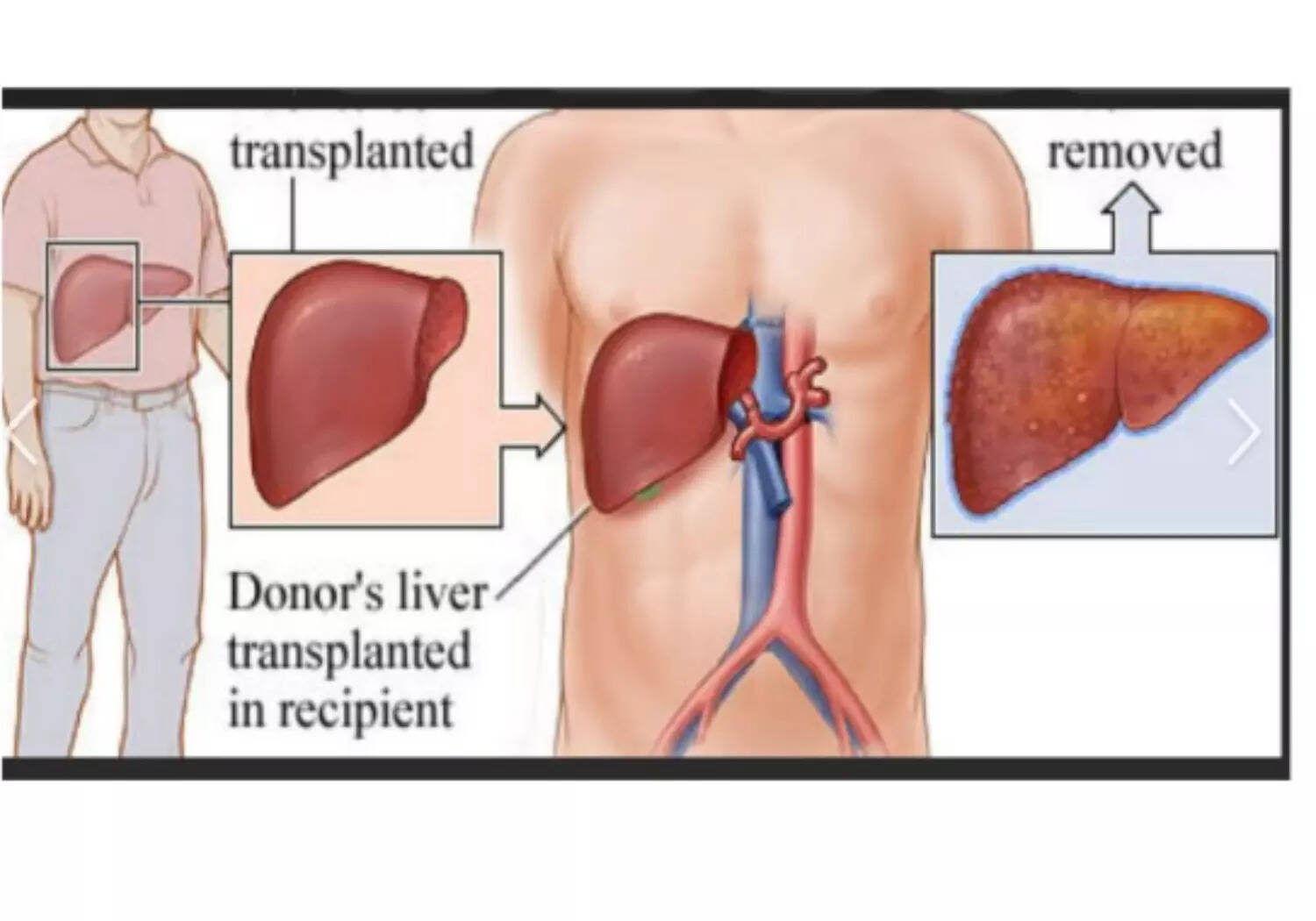
Shortage of organs (secondary to abysmally low organ donation rates) has led to the development of living donor programs in India (unlike west). Robust volumes drive strong performances & therefore it goes without saying that Indian transplant community has managed to deliver excellent results on global stage both in terms of donor & recipient outcomes.
The guiding principle in living donor transplants work on the “principle of double equipoise” which says the risk to the donor must be balanced with the benefits to the recipient. It essentially means the risk to the live donor must be kept minimum and the benefits to the recipient should be aimed at the maximum.
Therefore, it’s of vital importance to assess and develop protocols to improve live donor safety. Most centres dealing with live donor organ transplantation have stringent donor selection criteria to prevent adverse events and yet once in a while mishap have been reported. The ability of liver to regenerate quickly within few weeks make the living donor liver transplant option feasible and safe. Plus, shortage in cadaveric donor pool has also prompted living donor option especially in emergency situations (like sudden acute onset liver failure) and liver cancer patients where waiting may not be an option.
Strict regulation, guidelines and criteria for allocation of cadaveric organs restrict the indications of liver transplant in certain situations where mild extension of the criteria may actually translate into long term survival of the patient (recipient). Since living donor option is considered as a private property of the particular patient, cadaveric organ donor rules don’t apply to living donor scenario. In fact the ability to save an organ from cadaveric pool, no waiting time (therefore low waitlist mortality or death) and extension of the criteria (or indication) makes the living donor option very attractive. It is therefore extremely critical to make sure the safety of the live donor is given the priority.
The data from India is scarce on this issue given the fact that we are amongst the top 5 nations in the world in the field of living donor liver transplant. There is a lot of reluctance and insecurity regarding the public display of donor morbidity outcomes. Recently the team of doctors led by Dr Sable from Mumbai published the study which concludes and supports the previous observations that donor operations are safe in terms of low morbidity and zero mortality. However, there are certain caveats to the findings. The quality & percentage of the remaining liver must be good (non-fatty) and adequate (more than 30 per cent remnant). The team performing the live donor operation should have enough experience with the living donor surgery.
The authors have studied a total of 177 donors who underwent donor surgery (which included right & left liver lobe donations) and found that none of the donors developed complications which are grade IV (includes long term disability) or V (death). The study also points to the fact that approximately less than one fifth (1/5) donor will have some minor issues which can be managed medically and doesn’t affect the long-term outcomes of the donor. Dr Sable observed an interesting finding, which the study reported is that majority of the live donors are female gender (approximately more than 60 per cent) that includes wife, mothers, daughters or sisters.
Similar observations have been made in the past by other authors too. The most likely reasons could be due to social biases like patriarchal views, financial dependency, undue duress or coercion by family, fixed notion on gender roles etc. Donor advocacy may play an important role to mitigate some of the problem along with change in the societal mindset. It’s very important to emphasis the fact that the donor don’t need such a major surgery and yet is willing to undergo the operation in order to save his/her loved ones. Purely from decision making view point the recipient (or patient) outcome (survival rates) should be aimed at more than 90 per cent against the risk to the donor (approximately 0.2-0.5 per cent risk to life).
As per the THOA act, the donor should be close relative of the patient (preferably 1st degree), blood group matching or compatible (HLA matching not required), must be healthy (no medical or surgical illness) and most importantly mentally fit (& willing to donate). Dr Sable & his team had previously published on liver regeneration in live liver donors and concluded that healthy donor can donate up to 60 per cent of the liver safely in view of its regenerative potential and concluded that the remnant or remaining liver grows back to almost 80-90 per cent of its original size in merely 4-6 weeks.
“The only surest way of safeguarding our live donors is by generating (or donating) enough cadaveric organs to meet the growing demands, totally abolishing the need for live donation " concluded Dr Sable.
The article is written by Dr Shailesh Sable, an expert in liver transplantation, Jaslok Hopsital & Research Centre, Mumbai.
(DISCLAIMER: The views expressed are solely of the author and ETHealthworld.com does not necessarily subscribe to it. ETHealthworld.com shall not be responsible for any damage caused to any person/organisation directly or indirectly)


COMMENTS
All Comments
By commenting, you agree to the Prohibited Content Policy
PostBy commenting, you agree to the Prohibited Content Policy
PostFind this Comment Offensive?
Choose your reason below and click on the submit button. This will alert our moderators to take actions