- Industry
- 3 min read
Anaesthesia administration prior to breast cancer surgery can improve survival rate: TMC study
The results of this trial show that this simple, low-cost intervention significantly and substantially increases the cure rates and survival with a benefit that is ongoing for several years after surgery. The injection requires no additional expertise, is inexpensive, and can result in saving up to 100,000 lives annually globally. These benefits are substantial and were achieved with an intervention the cost of which was less than Rs 100 per patient.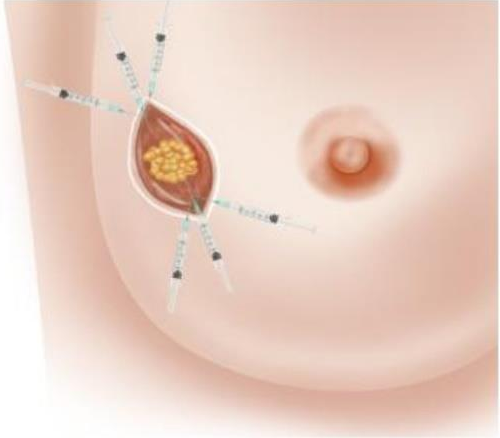
The clinical trial is an important milestone in the treatment of breast cancer. The trial in women undergoing breast cancer surgery involved the injection of a commonly used drug around the tumour on the operating table, just prior to surgery. The results of this trial show that this simple, low-cost intervention significantly and substantially increases the cure rates and survival with a benefit that is ongoing for several years after surgery. The injection requires no additional expertise, is inexpensive, and can result in saving up to 100,000 lives annually globally. These benefits are substantial and were achieved with an intervention the cost of which was less than Rs 100 per patient.
The study, ‘Effect of Peri-tumoural Infiltration of Local Anaesthetic Prior to Surgery on Survival in Early Breast Cancer’ is a randomised controlled trial, conceived and designed by Dr Badwe, who is the principal investigator. The study was conducted by investigators at 11 cancer centres in India including Tata Memorial Centre in Mumbai over an 11-year period between 2011 and 2022.
Joining from Paris immediately after his presentation, Dr Badwe commented, "For scientists, it opens the window of peri-operative intervention to modulate the environment of cancer in such a way as to prevent its deleterious reaction to the act of surgery [observation].
Dr Sudeep Gupta, Professor, Medical Oncology, TMC and Director, ACTREC, one of the co-investigators of the study said, “This study provides an inexpensive and immediately implementable treatment in breast cancer which can be practiced by every surgeon who treats this disease. The results from a large randomised trial, which is the gold-standard way of evaluating the worth of new treatments, provides the highest level of evidence to support the use of this technique.”
The study included 1600 women with early breast cancer who were planned to be treated with surgery. Half of these patients constituting the control group, received standard surgery followed by standard post-operative treatment including chemotherapy, hormone therapy and radiotherapy as per guidelines. The other half, constituting the intervention group, received an injection of a commonly used local anaesthesia agent, 0.5 per cent lidocaine, all around the tumour, just prior to surgery. They then underwent standard surgery followed by the same post-operative treatment as was given in the control group.
Dr Badwe’s previous research has suggested that there is a window of opportunity just prior to, during, and immediately after surgical removal of the primary cancer when anti-cancer interventions could reduce the risk of development of disseminated stage 4 metastatic cancer later in the lifespan of the patient. Lignocaine, which is a commonly used, inexpensive, local anaesthesia drug, was thought to be one such suitable intervention because of its inhibitory effects on cancer cell division, movement and other anti-cancer properties.
After completion of treatment patients were followed up regularly for several years to compare the rates of cure and survival between the control group and local anaesthesia group. When enough follow-up had happened in both groups the data was analysed at a cut-off date of September 2021. As expected, there was no toxicity of lignocaine in patients who received it. The 6-year disease-free survival (cure rate) was 81.7 per cent in the control group and 86.1 per cent in the local anaesthesia group for a 26 per cent relative reduction in the risk of cancer relapse or death with the local anaesthesia injection, which was statistically significant. Similarly the 6-year overall survival was 86.2 per cent versus 89.9 per cent in the two groups for a 29 per cent reduction in the risk of death with the local anaesthetic injection, which was also statistically significant.


COMMENTS
All Comments
By commenting, you agree to the Prohibited Content Policy
PostBy commenting, you agree to the Prohibited Content Policy
PostFind this Comment Offensive?
Choose your reason below and click on the submit button. This will alert our moderators to take actions